Fertility Fundamentals lays the foundations for understanding your reproductive health and empowers you to take control of your wellbeing. Reliable scientific information underpins everything we do and helps you go forward with confidence during your fertility journey.
Male Fertility
Understanding how your fertility functions means you are in the best place possible to help yourself if you encounter problems on your fertility journey. In this section, we lay down the basics of how fertility works in men and take a closer look at:
- The journey of a sperm cell
- Sperm production
- The semen analysis
- The process involved when you have a semen analysis
- The WHO criteria for semen analysis
- What has an impact on male fertility?
- Environmental effects
- How common is male infertility?
The journey of a sperm cell
For a single sperm to make it to an egg is the rough equivalent of a human being swimming around 2KM through a shark-infested thick soup with the currents of a swirling ocean to finally reach a treasure chest (that needs unlocking!) in an underwater cave – all without prior fitness training. It’s quite an incredible feat.

Sperm cells measure on average around 103µm in length (0.00000103cm – tiny!) and they have to swim over a thousand times their own body length to reach an egg. Most don’t make it that far. Of the millions of sperm in a normal ejaculate, only a few hundred reach the fallopian tube. They swim at speed first through the cervix, then up the uterus and, finally (for some), into the fallopian tube, enduring the changing environments of different parts of the female reproductive tract along the way.
They first encounter the hostile, acidic pH of the vagina before passing through the cervix, where they face the cervical mucus challenge – a day or two late and the oestrogen-induced slippery fertile mucus that allows the passage of sperm is gone, to be replaced by a thicker mucus brought on by increasing progesterone following ovulation, a mucus that is difficult for sperm to penetrate.
If timing is right and they do progress, the sperm cells then enter the uterus to face the biochemical army of an immune response and varying “currents” of the uterine fluid. Once inside the uterus they have to find their way through the two tiny openings (ostia) which allow passage from the uterus into the fallopian tubes, where, all being well, one should find and fertilise the egg.
 It’s no wonder, then, that sperm quality is needed for good fertility: it’s survival of the fittest. Sperm are also the only cells that are “designed” to function outside the human body, and the success of these unique cells involves a number of tightly controlled regulatory processes that all need to work well in order to produce a high number of cells with the right shape that can also swim well and fast. By facing the challenges of a hostile environment in order to reach the egg, most sperm cells are eliminated along the way and never reach their intended target. This means only the best quality sperm will reach the egg and, indeed, it is the swimming ability of sperm that allows an embryologist to select a sperm for ICSI when needed for male factor fertility issues. You can find out more in our online fertility courses.
It’s no wonder, then, that sperm quality is needed for good fertility: it’s survival of the fittest. Sperm are also the only cells that are “designed” to function outside the human body, and the success of these unique cells involves a number of tightly controlled regulatory processes that all need to work well in order to produce a high number of cells with the right shape that can also swim well and fast. By facing the challenges of a hostile environment in order to reach the egg, most sperm cells are eliminated along the way and never reach their intended target. This means only the best quality sperm will reach the egg and, indeed, it is the swimming ability of sperm that allows an embryologist to select a sperm for ICSI when needed for male factor fertility issues. You can find out more in our online fertility courses.
An incredible synchrony between man and woman is also needed for fertilisation to happen. A successful journey to reach the egg requires a two-way interaction between the female reproductive tract and the sperm. The environment inside the uterus modulates sperm function as it passes through and the female reproductive tract is altered by seminal fluid. Recent research shows that the egg releases chemical signals that attract particular sperm over others. These chemicals come from the follicular fluid that is released along with the oocyte at the time of ovulation and they increase the chance of fertilisation occurring. What is interesting is that it seems eggs may select sperm that is more genetically compatible, meaning that partner compatibility at a genetic level may be a factor in the fertility of a heterosexual couple where sperm and egg meet inside the body. The same could apply during IVF when sperm and egg meet in a petri dish.
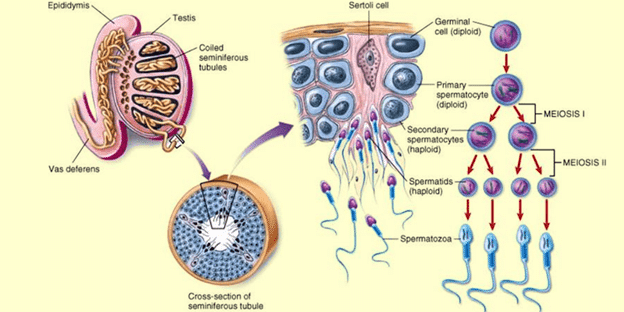
Sperm production
Sperm is continually formed in the testes in a process called spermatogenesis, which lasts approximately three months. Unlike women’s eggs, men’s sperm are not as old as they are and newly produced sperm is only ever three months old. Male fertility does also decline with age but to a lesser degree. The decline is also much less clear with men but includes a longer time to conceive generally, more losses due to things like miscarriage, greater need for ICSI during fertility treatment and lower chance of success with IVF for men older than 50. It also depends on the age of the female partner or egg donor as a younger woman’s eggs can correct sperm defects during early embryonic development.
Cells in the testis known as germ cells (cells that produce gametes – that is sperm and egg cells) divide all the time. This means there is a constant production line that supplies a reservoir inside the testes called the epididymis. Because of this continuous production, sperm soon start to die off to be replaced with fresh sperm. After a few days, they release chemicals as they degrade and these chemicals can adversely affect newly produced sperm. Long gaps between ejaculations can therefore impact sperm health as the dying sperm reduce the overall fertility of the sperm stored in the epididymis. The optimum interval between ejaculations is two to three days and so ideally a couple should have regular intercourse from the end of the menstrual bleed and throughout the fertile window (see The Fertile Window in our fertility guide). This is why it is important not to become too fixated on the fertile window and ovulation and restrict intercourse to these times as it may actually compromise your ability to conceive.
Diagram of male anatomy and sperm
Semen analysis
If you haven’t conceived after regular intercourse for a year, one of the important early investigations for a heterosexual couple is a semen analysis via your GP. This will tell you whether male factors are contributing to this delay. It is important for both of you to be investigated to ensure your fertility as a couple is assessed. Knowing there are problems with female fertility, for instance, should not mean you do not have the appropriate male investigations.
The process
In order to have a semen analysis, a man has to produce a sample by masturbation into a clean, dry container. The sample need to get to the lab within 30 minutes – most fertility clinics have private rooms on site, so samples can be assessed quickly. It’s important to abstain from ejaculation for 3 days before the test.
Sperm counts and motility in different samples from the same healthy, fertile man can vary significantly, so be cautious about relying on results from a single test. It’s best repeated on two or more occasions, ideally 3 months apart. In most cases, two semen analyses will be enough. Because sperm production takes 10–12 weeks, results give a picture of how well the testes have been working in the last 3 months. Bad results can improve over time and, equally, a good result can worsen if there are negative changes in diet and lifestyle.
Although the link between male fertility and results from a semen analysis are not always clear (it only takes a single good sperm cell to reach the egg from an ejaculate of millions!), the chance of natural conception falls significantly when the motile sperm concentration is less than 5 x 106/ml. When the total count is low there is often a corresponding reduction in motility. The concentration of progressively motile sperm consistently appears to be the most predictive factor for fertility.
The WHO criteria for the semen analysis
| Semen parameters | |
|---|---|
| Standard tests | Lower reference limit (95% confidence interval) |
| Volume | ≥ 1.5 ml (1.4 – 1.7) |
| pH | 7.2–8.0 |
| Sperm concentration | ≥ 15 x 106/ml (12 – 16) |
| Total sperm count | ≥ 39 x 106/ejaculate (33 – 46) |
| Motility (within 60 min of ejaculation) |
≥ 25% with rapid progression (category ‘a’) |
| ≥ 40% with forward progression (38 – 42) (categories ‘a’ and ‘b’) | |
| Vitality | ≥ 75% live (categories ‘a’, ‘b’ and ‘c’) |
| < 25% dead (category ‘d’) | |
| Morphology | ≥ 4 % normal forms (3.0-4.0) |
| White blood cells, a sign of infection | < 1 x 106/ml |
| Antisperm antibodies | < 50% |
What has an impact on male fertility?
Other parameters that can impact male fertility and that can be assessed via specialist tests include:
- Oxidative stress
- DNA fragmentation – damage to the DNA in sperm
Finally, epigenetic changes can also affect male fertility, though these are not usually analysed outside academic research. These factors and what you can do about it are covered in our online fertility courses.
If results from a semen analysis are poor, it is important to ensure you have the necessary medical investigations to rule out problems. We cover what happens medically on your fertility journey in our book, The Fertility Book: Your Definitive Guide to Achieving A Health Pregnancy.
Environmental effects
Because sperm is constantly being turned over in the testes, it is very responsive to lifestyle factors such as diet, exercise, environmental toxins, excess alcohol and smoking. All of these things can affect the parameters that are tested in a semen analysis and a good score does not guarantee overall sperm health and likelihood of conception.

Other factors that are actually more associated with IVF success that are not routinely tested include DNA damage, epigenetic changes and oxidative stress. Equally, a poor score on a semen analysis does not preclude getting pregnant, but does mean it’s likely it will be more difficult and indicates that there are underlying problems. It only takes one good sperm from an ejaculate of millions to fertilise an oocyte, so the link between male fertility and sperm quality and quantity is a not well understood. Sperm factors that impact IVF success can, however, be improved by dietary and lifestyle factors and whilst this certainly isn’t the only story when it comes to male infertility, we always recommend working together as a couple to achieve the best outcome.
How common is male infertility?
Given the level of performance needed for a sperm cell to successfully reach an egg, it isn’t surprising that male factor contribution to difficulty conceiving is significant. In terms of the burden of infertility, data suggests that around one in three cases of subfertility is solely male factor. Approximately one in three is a combination of male and female factor. This means that up to two-thirds of cases therefore involve male factor that is currently untreated.
These days, the only medical treatment for male factor infertility is IVF or ICSI, meaning that women have to undergo invasive medical treatment that carries a degree of risk and side-effects sometimes for reasons that have nothing to do with her own health. There is also growing evidence that paternal diet and other environmental factors impact not only sperm quality, but also early embryonic development, overall pregnancy outcomes and the health of the baby through into adulthood. It is therefore vital to understand what can be done to address the underlying causes of male as well as female fertility issues in order to optimise sperm health even for healthy men.
If the fertility of the couple is thoroughly assessed in this way, it may reduce the need for medical intervention, increase the prospect of treatment success where needed and protect the health of the baby. Of course, there are medical conditions that need treatment and underlying genetic factors that can’t be changed, so it is vital for all men to have a thorough medical investigation, but for all cases where a male partner is providing the sperm (rather than donor sperm), it is worth optimising diet, nutrient status and underlying health to put you in the best place possible for a successful outcome. You can find out more about evidence-based factors that can improve sperm quality in our online fertility courses.
References
- Adam Balen and Grace Dugdale. The Fertility Book: Your Definitive Guide to Achieving a Healthy Pregnancy. Penguin Random House (Vermilion) 2021
Copyright © 2024 Balance Fertility