Fertility Fundamentals lays the foundations for understanding your reproductive health and empowers you to take control of your wellbeing. Reliable scientific information underpins everything we do and helps you go forward with confidence during your fertility journey.
Female Fertility
Whether you’re trying to conceive now or planning a pregnancy in the near future, it helps to have an understanding of how your fertility functions, so you are in the best place possible to help yourself. In this section, we lay down the basics of how fertility works in women and take a closer look at eggs and hormones.
- Eggs and fertility
- The science of female fertility
- The egg store – ovarian reserve
- Loss of eggs over time
- Creating Eggs and Sperm
- Eggs and environment
- Hormones

Eggs and fertility
Girls are born with a fixed number of eggs that are formed as a baby develops in the mother’s womb. These eggs are continuously lost throughout your fertile years even if you are on your period or on the pill. As well as decreasing in number with age, egg quality also goes down as you get older. This is the same for all the cells in the body and part of normal ageing. Interestingly, egg quality is the main thing that influences IVF success and you can find out more about what you can do to improve egg quality from our courses. So, although IVF can help a bit when it comes to age-related fertility problems, in reality, it only really buys you a year or so. This is important to note, as many people believe that IVF can fix almost everything. It can’t.
Lifestyle factors can impact the ageing of all cells, including eggs, including the decline of fertility with age, so the earlier you start to adopt healthy behaviours, the more you will be able to influence your reproductive health over time and potentially extend your fertile years.
The science of female fertility
 Human egg cells are formed inside a female fetus during pregnancy and reach a certain point of maturity until development is halted. Eggs sit in the ovary in a state of suspended animation throughout childhood. When a girl reaches puberty and starts to menstruate, dormant follicles (the fluid-filled sacs inside which egg cells are held) are “chosen” out of the hundreds of thousands of egg cells to be the ones that re-start the development process in that particular egg. This takes several months from start to finish, with the completion of maturation (the “ripening”) taking about three months – a period that is important for egg quality in terms of diet and lifestyle. The “chosen” follicle grows to about 2cm in diameter and then releases its egg, which then passes into one of the fallopian tubes.
Human egg cells are formed inside a female fetus during pregnancy and reach a certain point of maturity until development is halted. Eggs sit in the ovary in a state of suspended animation throughout childhood. When a girl reaches puberty and starts to menstruate, dormant follicles (the fluid-filled sacs inside which egg cells are held) are “chosen” out of the hundreds of thousands of egg cells to be the ones that re-start the development process in that particular egg. This takes several months from start to finish, with the completion of maturation (the “ripening”) taking about three months – a period that is important for egg quality in terms of diet and lifestyle. The “chosen” follicle grows to about 2cm in diameter and then releases its egg, which then passes into one of the fallopian tubes.
It is in the fallopian tube where the egg meets sperm and where fertilisation happens. The newly fertilised egg is now an embryo and, at this first stage of development, is called a zygote. It represents the first stage of a new genetically unique individual where the genes of the parents combine. Following fertilisation, the embryo travels down the fallopian tube into the uterus, where it implants into the lining of the uterus (endometrium) and grows as a pregnancy. If fertilisation does not happen, or if the embryo fails to implant, the endometrium falls away as a menstrual period about 14 days later.
The egg store – ovarian reserve
 You are born with more eggs than you will ever need (an amazing 1-2 million!) and the number declines throughout childhood and the fertile years. By the time ovulation first happens and your periods start around the age of 13, there are about 400,000 eggs left. At the menopause stage, which is on average around the age of 51, there are no eggs left to be ovulated.
You are born with more eggs than you will ever need (an amazing 1-2 million!) and the number declines throughout childhood and the fertile years. By the time ovulation first happens and your periods start around the age of 13, there are about 400,000 eggs left. At the menopause stage, which is on average around the age of 51, there are no eggs left to be ovulated.
If you ovulate one egg each month during your fertile years, that would be equivalent to the release of only around 456 eggs (even if you ovulated each and every month, which doesn’t always happen). Ovulation doesn’t become regular for a year or two after puberty, for instance, and ovulation stops during pregnancy, breast feeding and the use of certain contraceptives. Despite this, the number of eggs progressively and relentlessly declines.
We now know that during a woman’s twenties maybe 1,000 eggs are lost each month. That’s 30 every day that are simply wasted! The monthly loss of eggs goes down with age to maybe 100 per month in her late thirties. This steady decline is not under the influence of hormones but instead due to inbuilt signals in the ovaries and the eggs themselves. It’s around the age of 37 years when the decline becomes more rapid until the menopause.
Loss of eggs over time
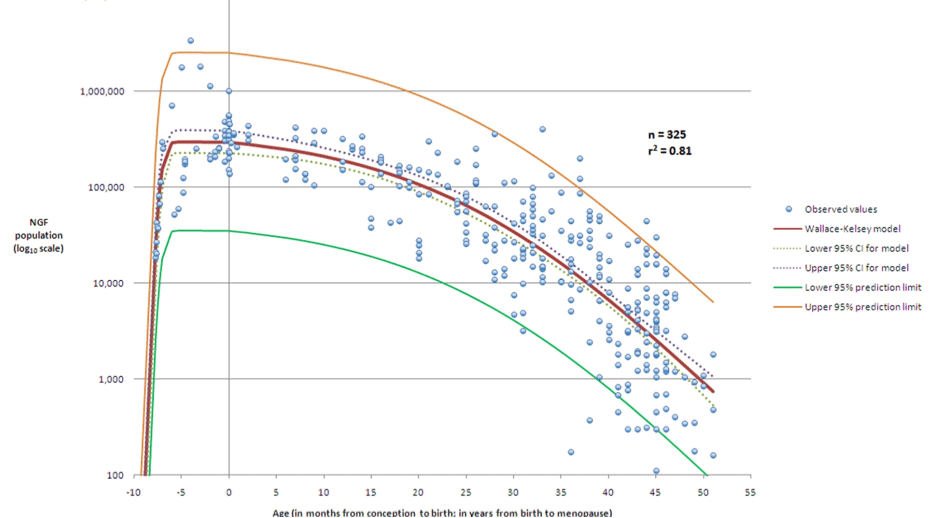
The Y (vertical) axis shows the number of eggs and the X (horizontal) axis shows female age from before birth through to menopause.
Creating Eggs and Sperm
Cells divide in two ways. One way creates a copy of the “mother” cell resulting in the full number of chromosomes in the ”daughter” cell. This form of cell division is called mitosis and it is the way that cells making up the bulk of our bodies are produced. Cells including muscle, heart, kidney, lung, bone, hair, teeth and skin are produced in this way and are called somatic cells, which essentially means normal body cells. The other type of cell division results in half the number of chromosomes in the “daughter” cell – meiosis. Meiosis is the type of cell division that produces sperm and eggs – collectively known as gametes. Both sperm and eggs have 23 chromosomes and, when an egg is fertilised, the correct number of chromosomes for human cells is restored when the sperm and the egg join their genetic material together. So a healthy adult human has 46 chromosomes (22 pairs numbered 1 to 22 and then either two X chromosomes in females or an X and Y in males).
Eggs and environment
This means that the period during which eggs are awakened from their inactive state to complete the process of cell division (meiosis) and the eggs mature, is especially important for egg quality. The environment in which this happens and also maternal age impacts how well the final processes of meiosis work. So, although our diet and lifestyle generally have an impact on our fertility throughout our life, the months leading up to conception are some of the most important in terms of our capacity to produce the best quality eggs our body is capable of producing for our age. This is one reason why the preconception period is so critical, which we cover in our courses.
Because egg cells or oocytes are as old as a woman and remain inside her throughout life until the menopause, they are subjected to the same environmental exposures as the individual woman. So, what a woman does throughout her life has an ongoing impact on her fertility and the health of her eggs. Every cigarette, glass of wine, junk food meal and phase of couch potato inactivity provides a low-level drip-feed of damaging biochemical influences on the eggs and cells that surround them. These surrounding cells are involved in the processes that lead to maturation (the “ripening” of the egg) and ovulation (the release of the egg from the ovary each month).

 These influences have the potential to impact the egg and surrounding cells through many different mechanisms. Everything we do to our bodies impacts the tiny structures within a cell that produce the energy for all our bodily processes, known as the mitochondria (the “battery” of the cell), for instance. The same environmental factors also affect our genes (the bundles of DNA that provide the instructions for how are cells function) and whether or not they are “switched on” and fulfil their intended function in the body – this is epigenetics. These are two things that are important for many different areas of health, not just our fertility, and are some of the factors that we can influence through our behaviours and habits.
These influences have the potential to impact the egg and surrounding cells through many different mechanisms. Everything we do to our bodies impacts the tiny structures within a cell that produce the energy for all our bodily processes, known as the mitochondria (the “battery” of the cell), for instance. The same environmental factors also affect our genes (the bundles of DNA that provide the instructions for how are cells function) and whether or not they are “switched on” and fulfil their intended function in the body – this is epigenetics. These are two things that are important for many different areas of health, not just our fertility, and are some of the factors that we can influence through our behaviours and habits.
These factors can impact sperm health in a similar way, which we will cover in our courses.
Although we are still learning about the incredible way our diet and lifestyle impact our health and fertility, we understand enough to know very clearly the importance of these things when it comes to creating a new life. In this way, through our eggs (and sperm too), we are laying down the foundations for the future health of our children before they are even born. We hold incredible power, and having an understanding of how we can change what we do to our bodies for our general wellbeing as well as our fertility means we have power that previous generations have not had; power that we can use to protect the lifelong health of our children.
Hormones
Hormones, in the correct balance, are needed for conception and for a healthy pregnancy to develop. So in this section we look at the main hormones you might hear about when talking about fertility and the importance of ovulation in maintaining the hormone balance you need to have a baby. We will also look at the role of hormones in your menstrual cycle, and why a regular, healthy menstrual cycle is foundation for good fertility. We cover period problems and what that might mean for your fertility in our courses.
How your ovaries work
As well as producing and storing the eggs, the other main purpose of the ovary is to produce hormones. Hormones are substances that are released into the blood stream and circulate around the body to make sure all your organs and bodily processes are working as they should. They also have a big impact on behaviour (think sex drive and testosterone). The hormones from the ovary affect many different parts of the body, but especially the uterus and breasts. The hormones produced by the ovary fall into three main groups: oestrogens, androgens and progestogens. Women make all of these hormones, but sometimes in different proportions. Testosterone is sometimes seen as a male hormone but it is the main androgen hormone made by the ovaries of all women. Oestrogen is actually made out of testosterone and helps the lining of the womb (endometrium) to grow.
The menstrual cycle
The menstrual cycle is divided into four main phases and each phase is significant in terms of your fertility. Understanding your menstrual cycle will help you to understand when you are fertile (your fertile window) and to interpret results of any investigations you may need.
There are four stages of the menstrual cycle: follicular phase, ovulation, luteal phase and menstrual phase.

Follicular phase
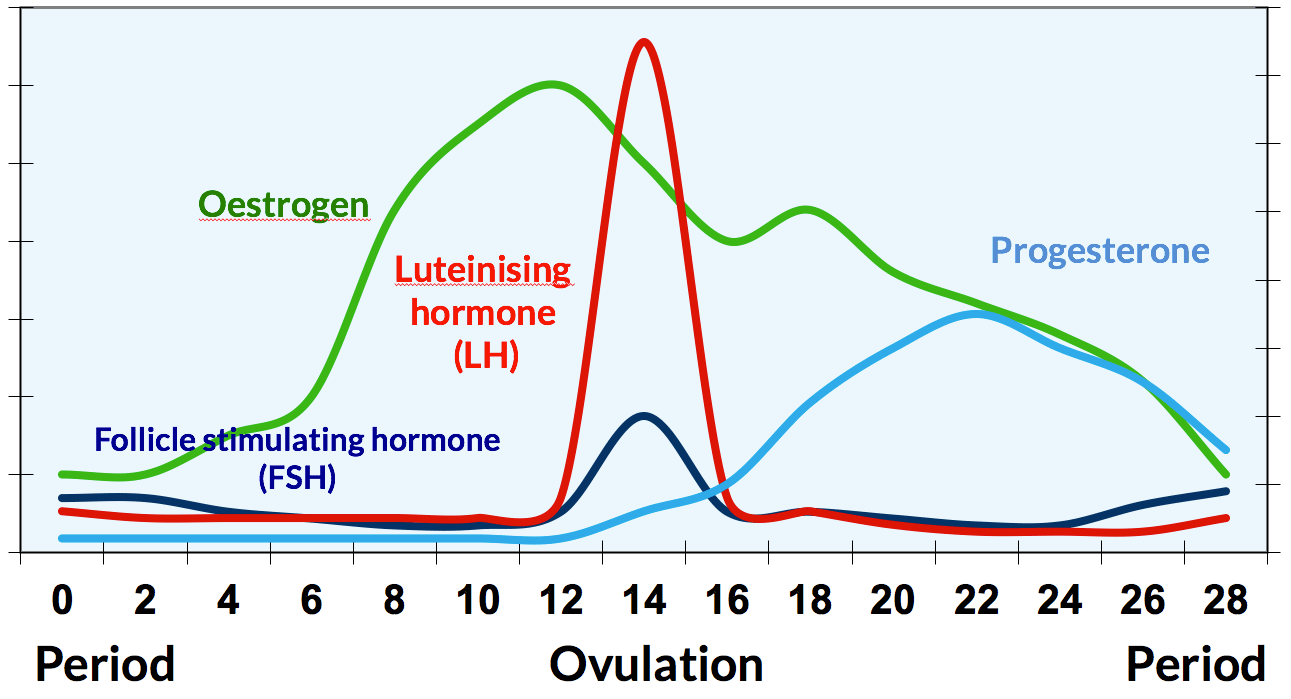
This is the phase of your cycle when the follicle that is going to release an egg that month starts to grow and produce other hormones that lead to ovulation. One important hormone involved is follicle stimulating hormone, or FSH. It’s produced by a gland at the bottom of the brain called the pituitary gland and it stimulates the growth of the follicle, peaking between days 3-5 of your cycle (the days in your cycle when it should be tested – our home testing service is coming soon). The FSH you produce naturally usually initiates the growth of just one follicle, but injections of FSH that are given during fertility treatment make it possible to stimulate the growth of others that otherwise would have died away. As a follicle grows it produces various hormones including oestrogen, and other hormones that effectively block the growth of other follicles. Oestrogen is the hormone that stimulates the growth of the endometrium.
Ovulation
Ovulation – the release of the egg from the follicle into the fallopian tube – is the main event of your menstrual cycle and the one that is crucial for natural conception. Ovulation happens because the growing follicle produces increasing amounts of oestrogen until it reaches a peak, where it triggers the release of a surge of another hormone called luteinising hormone (LH). LH is also produced by the pituitary gland. LH is the hormone that then starts the process of ovulation and also prepares the egg for fertilisation. Both the oestrogen peak and the LH surge are used to detect ovulation by some ovulation detection kits.
Luteal phase
 After ovulation, the follicle continues to produce oestrogen and it also starts to produce another hormone that is really important for a pregnancy to be sustained if the egg is fertilised. That hormone is progesterone. Progesterone usually peaks around a week before your next period (eg day 21 of a 28 day cycle) and is tested by GPs around this time to check you are ovulating. Measuring it on the wrong day of your cycle often happens and this can be very misleading. Whilst oestrogen stimulates the growth of the endometrium, progesterone is the hormone that gets the endometrium ready for the implantation of the embryo. Progesterone also helps maintain the endometrium after implantation and so adequate levels are needed for a pregnancy to continue. We will cover factors that can affect the all-important balance between these two hormones in our courses.
After ovulation, the follicle continues to produce oestrogen and it also starts to produce another hormone that is really important for a pregnancy to be sustained if the egg is fertilised. That hormone is progesterone. Progesterone usually peaks around a week before your next period (eg day 21 of a 28 day cycle) and is tested by GPs around this time to check you are ovulating. Measuring it on the wrong day of your cycle often happens and this can be very misleading. Whilst oestrogen stimulates the growth of the endometrium, progesterone is the hormone that gets the endometrium ready for the implantation of the embryo. Progesterone also helps maintain the endometrium after implantation and so adequate levels are needed for a pregnancy to continue. We will cover factors that can affect the all-important balance between these two hormones in our courses.
Menstrual phase
If the egg is not fertilised, it starts to break down and progesterone and oestrogen then fall. Without the hormones needed to maintain the endometrium, the lining itself starts to break down and this is your menstrual period.
Your body then enters into a new monthly cycle where the whole process starts all over again.
A normal menstrual cycle
The graph below shows the changes in hormone levels across the cycle and you can see that oestrogen (green line) peaks just before the LH surge (red line). You can also see why measuring progesterone (blue line) on the wrong day of the month could be very misleading and make you believe you have low progesterone when you haven’t. When you have blood tests matters!
References
- Adam Balen and Grace Dugdale. The Fertility Book: Your Definitive Guide to Achieving a Healthy Pregnancy. Penguin Random House (Vermilion) 2021
Copyright © 2024 Balance Fertility